Living With AMD
Meet Cherie, who explains her experience with anti-VEGF injections for AMD
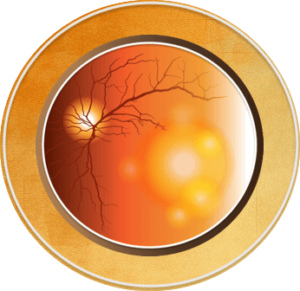
It is possible to have age-related macular degeneration (AMD) without any symptoms. People with early and intermediate stages of AMD rarely notice any symptoms; in comparison, people with severe dry or wet AMD usually notice symptoms. Symptoms of AMD may occur in one or both eyes and include:1-5
- Reduced vision
- A blind or blurry spot in the vision
- Faded color vision
- Visual distortion
- Difficulty with low light situations
AMD is a progressive disease, meaning symptoms usually get worse over time. When visual changes occur, AMD is most likely intermediate to severe disease. Early detection and referral to an ophthalmologist is important because monitoring and early initiation of treatments to help slow down the progression of intermediate to severe AMD, as well as preserve central vision in wet AMD, can be given.1-5.
Not everyone with AMD develops severe AMD or gets it in both eyes. For those who do, activities that require fine visual acuity, such as driving or reading are harder to do. Using assistive devices, such as brighter lights or a magnifying lens for specific tasks, can help improve everyday activities. Vision rehabilitation specialists can help with learning to live with vision loss, with training on how to use magnifying devices or apps for reading, guidance on home set-up to move around easily, and sharing resources to help cope with vision loss.1-5
If you have early AMD or a family history of AMD, you may be given an Amsler grid to check your vision each week. Test each eye by covering one eye at a time and reading the Amsler grid, noting any new vision changes, such as missing areas of the grid or distorted/wavy lines.5 Let your doctor know if you notice any changes.
References
- AMDF. Dry Age-related Macular Degeneration. https://www.macular.org/about-macular-degeneration/dry-macular-degeneration
- AMDF. Wet Age-related Macular Degeneration. https://www.macular.org/about-macular-degeneration/wet-macular-degeneration
- CDC. About Age-Related Macular Degeneration. Vision and Eye Health. May 15, 2024. https://www.cdc.gov/vision-health/about-eye-disorders/age-related-macular-degeneration.html
- Cunningham J. Recognizing age-related macular degeneration in primary care. JAAPA. 2017;30:18-22.
- Vemulakonda GA, Bailey ST, Kim SJ, et al. Age-Related Macular Degeneration Preferred Practice Pattern®. Ophthalmology. 2025;132(4):P1-P74.
All URLs accessed June 26, 2025.